Support quality, independent, local journalism…that matters
From just £1 a month you can help fund our work – and use our website without adverts. Become a member today

Deri Medical Centre is set to close after the health board supported an application from the main practice to shut the branch
Meddygfa Cwm Rhymni, which runs the branch, applied to Aneurin Bevan University Health Board (ABUHB) to close its surgery at Riverside Walk, Deri, back in early 2023.
Following an eight-week engagement period, a vacant practice panel opted to close the site – a decision that was formalised at ABUHB’s public board meeting on July 19.
Speaking at the public board meeting, ABUHB’s chief operating officer, Leanne Watkins, said: “The recommendation of the panel, and also supported from an executing perspective in June, is that we support the request for branch closure in the interest of sustainability.”
What is a Vacant Practice Panel?
Access to general medical services is the responsibility of the health boards when a doctor or doctors at a practice resign their contracts.
When a health board receives a general medical services (GMS) contract resignation, it then instigates the vacant practice process.
This process will include representatives who will consider the options available for the future provision of that practice.
Options that can be considered include: advertising the practice, allocating patients to local GP practices, and the health board assuming management of the practice.
As a branch surgery, patients are registered with the main practice – Meddygfa Cwm Rhymni. There are 12,800 registered patients, of which 777 patients accessed services at the Deri branch, according to a supporting document provided at the board meeting.
These patients will now need to permanently use other sites in New Tredegar or Rhymney.
Staff who work at the Deri branch will also relocate to either the New Tredegar branch or the main practice in Rhymney.
Nearly 90% of patients attended the branch
The application to close the branch surgery prompted an eight-week engagement period with patients, which started on March 20.
Letters and questionnaires were sent out to patients aged 16 and over who accessed services at the Deri branch, asking for feedback on the closure.
Of those 673 patients aged 16 and over, 105 completed online responses and two paper questionnaires were received by the closing date of May 22. An additional 62 responses were also received from patients who had devised their own questionnaire.
Feedback in person was also an option, however, speaking in the public board meeting, CEO Leanne Watkins said: “Only 11 patients actually attended in person for that.”
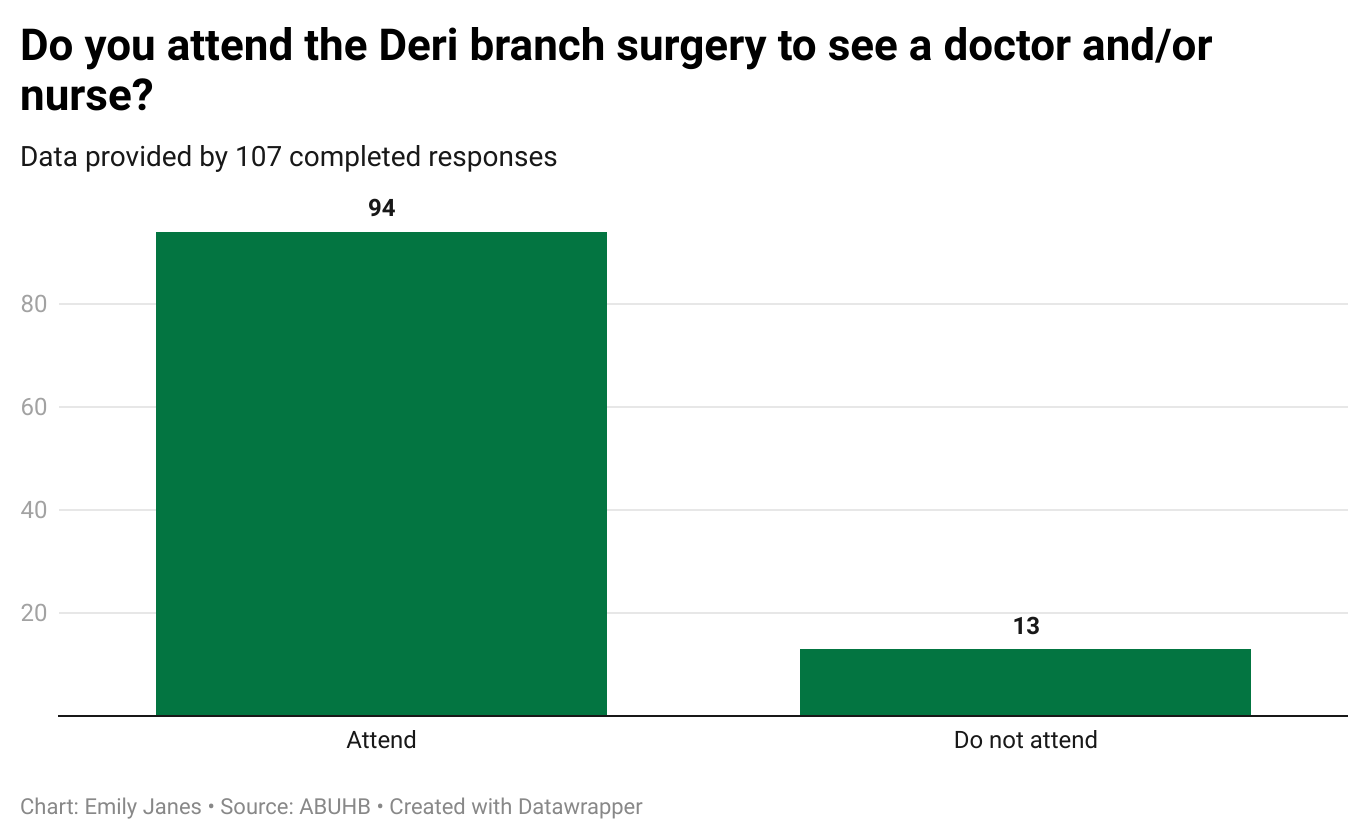
Of the 107 responses, 88% of patients said they attended the branch surgery – only 12% did not. Whereas, 53% of respondents said they attend the main surgery at Rhymney to see a doctor or nurse.
However, speaking in the meeting, Ms Watkins noted that there was a lack of services offered at the Deri branch and said: “[Patients] aren’t able to give samples there, they can’t access allied health professionals, district nursing, all sorts of health visiting from that branch.
“It’s not a great offer for our patients even if they can have an initial consultation there,” adding that follow-up care is often required at other sites such as the one in Rhymney.
For the health board, this raised an issue of sustainability and utilising their workforce in the best way.
“We talk a lot about sustainability and utilising our workforce to maximum effect,” said Ms Watkins, “lots of those patients won’t be well served by that capacity either.”
There were also 20 individual comments received which largely focused on two points – that many patients thought the branch was closed or appointments there couldn’t be accessed and that travelling to other sites would be a problem because of unreliable public transport and taxi journeys, which could cost up to £20.
It was also noted that no Senedd Member or Member of Parliament had raised the closure of the branch.
‘Unsustainable’
The supporting document, Equality Impact Assessment (EqIA), provided to attendees of the board meeting gives a number of reasons for the closure.
It states that the Deri branch closure would allow the practice to consolidate its overall services and “support the delivery of the full range of services to the registered population.”
Providing services across three sites is described as “unsustainable” and complicated by the practice, having lost one GP and two practice nurses over the last few years.
Renovation works would also be needed at the site at an estimated cost of £123,000 – this was the number quoted when the site was surveyed by Oakleaf Group on behalf of ABUHB in 2019.
In the public board meeting, it was also mentioned that the lease was about to expire but Ms Watkins mentioned that a conversation had been had with the landlord “outside of the process”.
‘Our transport links are non-existent’
As part of the equality impact assessment in the supporting document, there was a point which echoed previous concerns about the elderly population of the area and a lack of transport options to access treatment in Rhymney or New Tredegar.
Cllr David Nicholas, who represents Deri and Groesfaen on Darran Valley Community Council, previously told Caerphilly Observer that the need to travel to access care of any kind was a worry for constituents and said: “It’s a very elderly village.”
He added: “Our transport links are non-existent.”
Part of the supporting document is the health board’s Equality Impact Assessment’s Scoring Chart, where positive scores are rated on a scale of minus-nine to nine. Nine suggests there will be a positive impact, minus-nine means a negative impact, while zero means no impact at all.
For the category of age, the closure of Deri surgery had the highest impact rating possible – scoring a minus-nine, meaning that it was classed as a “high impact” decision.
Ms Watkins said: “We have, just for assurance, also shared with Llais [the independent statutory body for health and social care] and the population some additional offers in relation to sort of potential access to transport, which I think is important given some of the health inequalities there.”
More change for Meddygfa Cwm Rhymni
The addition of patients from Deri is not the only change that is facing Meddygfa Cwm Rhymni.
The practice has also taken on patients from Lawn Medical Practice after doctors handed back their contracts.
This means that an additional 5,500 patients will be added to Meddygfa Cwm Rhymni’s current register of patients. This decision was also approved at ABUHB’s July public board meeting.
While Caerphilly Observer understands patients can still access services from the existing premises based in Rhymney Integrated Health and Social Care Centre, there have been concerns over staffing issues.
A spokesperson for ABUHB previously confirmed that staff from Lawn Medical Practice would be transferred to the new practice – this would not include GP partners, although “discussions may take place between the partners.”
Labour councillor Carl Cuss, who represents Twyn Carno, previously told Caerphilly Observer: “Residents will rightly want to know how the new surgery will deal with the extra capacity.
“I understand staff could be transferred but I think concerns around whether additional GPs are needed still need clarifying.”

This comes despite one of the reasons for Deri’s closure was down to recruitment troubles for Meddygfa Cwm Rhymni.
In fact, the loss of one GP and two practice nurses meant that there was already an “immediate deficit of ten GP sessions per week across all sites”.
During the public board meeting, one member asked how the changes would affect the “number of sessions per patient caused by those two sets of changes”.
Ms Watkins said that while this number was not immediately available it could be provided after the meeting.
She added that the vacant practice panels would have the additional patients from Lawn Medical Practice and Deri surgery into account and continued: “The conversation I’ve had with the team on this is that this is to support the sustainability and delivery of that larger practice.
“We can’t afford to have staff sat in a branch delivering care to three patients when it could be delivering to 20 or 30 or 40 a day, which is the norm
She added: “The panel has to provide that confidence that it’s got sustainable staffing to have awarded that contract and I’m confident and assured that they will have done that in that process.”
Support quality, independent, local journalism…that matters
From just £1 a month you can help fund our work – and use our website without adverts.
Become a member today
